A history of pandemics and our treatment of them.
The Cholera outbreak in the 1840’s had actually 7 pandemic phases. This we got from a bacterium called Vibrio cholerae. Symptoms were severe watery diarrhea, which can lead to dehydration and even death if left untreated. Cure was to drink good water with electrolytes.
We didn’t get an antibiotic for this until over a century later – 1964. (1928 penicillin was the 1st antibiotic, Alexander Fleming).
The earliest flu pandemic for which detailed records are available is the 1889 Russian flu, a.k.a. Asian Flu, but the name is a vague, as this flu originated in Bukhara, Uzbekistan. In the USA, it got the nickname, the Grippe, after the French nickname.
That traveled the world in 4 months when there were no planes. How? Railroad connections. 125,000 miles of train lines, more than we have today. Killed about 1 million ppl.
At the time, many different ideas for what caused the disease were postulated. Science at this time wasn’t great, and some doctors seriously considered earthquakes as the cause. Other theories held that electrical and magnetic phenomenon were “likely agents”. Others thought that electrical currents in the air could produce ozone, which intensified the illness.
(I mention this because some people today think the present virus comes from the 5G towers. 5G towers are a problem because the Chinese had planned to use them to spy on those countries where they were to be installed.)
Some of the continent’s most prominent leaders—the Tzar of Russia, the king of Belgium, the emperor of Germany—had fallen ill with the Asian Flu.
Americans weren’t worried about it – that pandemic was safely over there, a vast ocean away. It came to America in December, 1889, through the East Coast Port Cities – NY city.
Initially, public health officials played down the dangers, and in January, 1890, NY city has over 1,200 dead from the flu or its’ complications. Meanwhile, the disease spread inland, helped, as in Europe, by America’s vast network of railroads.
The flu eventually died off on its own, and the ppl who had it and survived also had the antibodies to fight off any recurring attacks.
This was the beginning of life — and death — in an increasingly interconnected world.
Pneumonia is an infection in one or both lungs. Bacteria, viruses, and fungi cause it. Bacteria based is the most common and can be treated with antibiotics. Viruses account for about one third of pneumonia cases and this is where you get the rhinoviruses and coronaviruses.
H1N1 viruses aren’t new. They’ve been circulating since at least 1918, when a new strain appeared simultaneously in pigs and humans and killed 40 to 50 million people in a single year. I say “at least” 1918, because this is the 1st time the illness is tracked.
It has never been clear where this pandemic began, because 1918 was also the beginning of WW1. World War I censors hid it to maintain morale in the armed forces. So, they didn’t report illnesses and death in Germany, England and France – but they could report on Spain, because Spain was neutral. Today some researchers believe that Haskell County, Kansas, is the likely source. There, the smell of manure meant civilisation, and ppl lived in sod houses. Prairie grass has a much thicker, tougher root structure than a modern lawn. They had houses made of dirt.
Haskell is 300 miles to the west of Funston, a military base. Many of the soldiers from Funston were sent over to Europe. They land in France – 1st outbreak in Europe is there. The 2nd wave of this virus was more dangerous, because the virus had mutated. And there was a 3rd wave, and there was a 4th wave.
This 1918 flu killed between 2 and 20% of those infected, as opposed to the more usual flu epidemic mortality rate of 0.1%.
It’s not until 1931 that we can identify that this flu is cause by a virus and not bacteria.
This virus came from the family Orthomyxoviridae, and was first discovered in pigs by Richard Shope. Isolating the virus in humans came in 1933. In 1935 they discovered that the virus wasn’t composed of cells. To understand the name, orthós, Greek for “straight”; mýxa, for “mucus”. It is a family of RNA viruses. It includes seven genera: Alphainfluenzavirus, Betainfluenzavirus, Deltainfluenzavirus, Gammainfluenzavirus, Isavirus (salmon), Thogotovirus (ticks and mosquitoes), and Quaranjavirus.
- A virus is a microscopic parasite. It is much smaller than bacteria – 8 times smaller is your minimum. You need a special, Electron microscope for that, which wasn’t invented until the 1930’s. The virus can only survive in a living host.
By the way, with the flu, a person is contagious from 1 day before symptoms appear and up to 5 days after becoming sick. It is responsible for about 36,000 human deaths and 200,000 hospitalisations every year in the United States alone.
- Influenza viruses are divided into three basic groups known as influenza A, B and C. Influenza A is the most common type, found in both animals and humans, and H1N1 is the 1st example found of influenza A.
To understand what H1N1 means, the “H” (hemagglutinin) and the “N” (neuraminidases) are proteins. They are found on the outer shell of the virus.
There are 16 (H1 to H16) known types of hemaglutinin.
There are 9 (N1 to N9) known types of neuraminidase, which gives 144 different possible combinations of these proteins.
It is not until 1940 that the first vaccine was created for the 1918 flu. This original vaccine only includes an inactivated influenza A virus. This same year, Influenza B viruses were discovered.
Influenza B almost exclusively infects humans and is less common than influenza A. Flu type B also mutates about two to three times more slowly than influenza A.
A protein labeled “M2” in influenza virus helps it multiply and also damages lung epithelial cells, causing fluid buildup in the lungs. M2 damages the protein responsible for clearing fluid from the lungs by increasing the amount of oxidants, or free radicals, within the cells. Oxidants are necessary for proper cell function, but can become toxic if uncontrolled. (Source: https://www.sciencedaily.com/releases/2009/07/090717150302.htm)
The World Health Organisation began in 1948. They say we’ve been living in a “pandemic era.” From 1918 to 1957, H1N1 viruses circulated every year as the seasonal flu. Then in 1957, a new flu virus, H2N2, appeared on the scene and H1N1 disappeared.
Asian Flu, 1957.
The Asian flu was a global pandemic of influenza “A” virus subtype H2N2 which originated in Guizhou, China and killed at least 1 million people worldwide.
The strain of virus that caused the pandemic was influenza A virus subtype H2N2, a combination of avian influenza (probably from geese) and human influenza viruses.
The first cases were reported in Guizhou in late 1956. By 1957 it was in the USA.
There was a first wave that peaked in October (among children who returned to school) and
There was a second wave, in January and February 1958 among elderly, which was more fatal.
This virus had an overall mortality rate of 0.6%, which is considered deadly.
This H2N2 influenza virus continued to circulate FOR 10 YEARS, until 1968, when it transformed via antigenic shift into influenza A virus subtype H3N2, the cause of the 1968 influenza pandemic.
Antigenic shift refers to an abrupt, major change that produces a new influenza subtype in humans that was not previously transmitted between people. It occurs through animal to human transmission or through mixing of human influenza ‘A’ and animal influenza ‘A’ virus genes to create a new human influenza ‘A’ subtype. This will have new types of hemaglutinin, neuraminidase or both.
To put it more simply, it is a genetic process in which genes from multiple subtypes are re-assorted and therefore form a new virus.
When this happens, most people have little or no protection against the new influenza virus, as was the case in the H1N1 virus.
The Hong Kong flu was a flu pandemic that took place in 1968 and 1969, and killed an estimated one million people all over the world.
This was caused by an H3N2 strain of the influenza A virus, descended from H2N2 through antigenic shift.
In 1994 there was a SARS (Severe Acute Respiratory Syndrome) outbreak in Australia called the Hendra virus. WHO doesn’t recognise this as a SARS, even tho the source and symptoms are the same: bats infected horses, people got it from the horses. The fatality rate is 60% in humans and 75% in horses. Symptoms of Hendra virus infection in humans range from mild influenza-like illness to fatal respiratory or neurological disease. A vaccine was developed for the horses in the year 2012 and finally approved in 2015.
A vaccine for humans was never developed.
To be technical, the Hendra virus, like Ebola, are members of different viral families. However, they both can and are treated as SARS (Source: https://pubmed.ncbi.nlm.nih.gov/24501399/).
2003-2004 Bird Flu. This is the 1st SARS virus that WHO recognises. Fatality rate of about 10%. Asian H5N1 viruses were first detected in domestic geese in southern China in 1996. By 2000, their host range had extended to domestic ducks, which played a key role in the genesis of the 2003/04 outbreaks.
Candidate vaccines were developed in the United States and the United Kingdom during 2003 for protection against the strain, but the 2003 strain died out in 2004 making the vaccine of little use.
2009-2010 Swine flu. Originated in pigs from a very small region in central Mexico. About 17,000 deaths worldwide. The 2009-2010 season was very unusual. The emergence of this new and very different H1N1 virus meant that two vaccines were needed: one to prevent seasonal influenza viruses that were anticipated to spread and another to prevent influenza caused by the newly emerged 2009 H1N1 virus.
MERS-CoV – 2012. Middle Eastern Respiratory Syndrome. 30-40% fatality rate. The first confirmed case was reported in Jeddah, Saudi Arabia in April 2012. The evidence available to date suggests that the viruses have been present in bats for some time and had spread to camels by the mid 1990s. The viruses appear to have spread from camels to humans in the early 2010s.
No MERS vaccines are available for human use.
SARS 2014. In late 2017, Chinese scientists traced the virus through the intermediary of Asian palm civets to cave-dwelling horseshoe bats in Yunnan. There is currently no proven antiviral therapy.
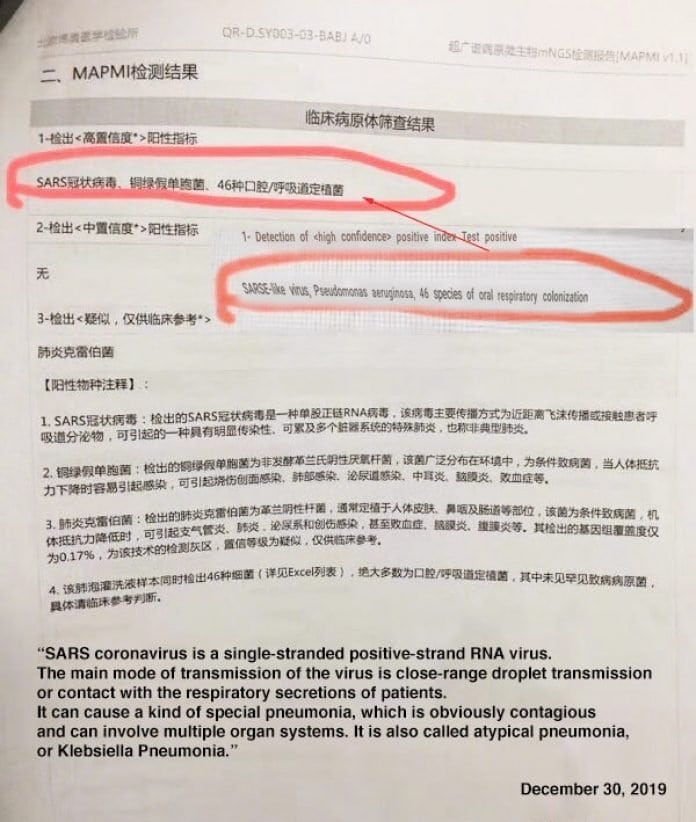
SARS Cov2 – 2019. Another article will be uploaded soon covering the controversial beginnings of this virus.